Common Breastfeeding Pain Questions and Solutions

You might have imagined breastfeeding as a warm, instinctive experience, a quiet moment between you and your baby. But instead, you feel sharp jolts of pain or a deep ache every time your baby latches. If you’re reading this, you’re likely caught in that confusing space between hope and worry, trying to understand whether what you’re feeling is normal or a sign that something isn’t quite right.
You’re not alone. Studies show that over 85% of women report experiencing some pain in the early days of breastfeeding as their bodies and babies learn to work together. That can take an emotional toll too, leaving you anxious, discouraged, or even questioning your ability to feed your baby.
In this blog, we will walk you through when breastfeeding hurts normally versus when it’s a sign that something isn’t right, the possible causes, and how professional support can make feeding easier.
Key Takeaways
- Some early tenderness is common, but ongoing or intense breastfeeding pain is not something you’re expected to tolerate.
- When breastfeeding hurts, it usually has a clear cause, and most discomfort can be relieved with the right adjustments and care.
- Small changes in latch, positioning, pumping, or breast care can make a noticeable difference in comfort.
- Lactation consultants help identify the source of pain and provide practical, hands-on solutions.
- Insurance often covers breastfeeding support and supplies, making professional help more accessible.
Is It Normal That Breastfeeding Hurts?
Let’s clear this up gently, because this is where a lot of worry begins. Some discomfort at the very beginning can happen, especially in the first few days when your body and your baby are still figuring things out together. You might feel tenderness, a stretching sensation, or brief sensitivity when your baby first latches. For many moms, this eases as feeds continue and positioning improves.
But here’s the important part: breastfeeding should not feel painful every time. Pain that makes you brace yourself, clench your teeth, or dread the next feeding isn’t something you’re expected to push through.
A helpful way to think about it:
- Early, mild discomfort that improves within the first week can be part of the adjustment phase
- Sharp, burning, stabbing, or worsening pain is your body’s way of asking for attention
- Pain that lasts beyond 1–2 weeks, causes cracked or bleeding nipples, or doesn’t improve with small adjustments deserves extra support.
If something feels off, trust that instinct. Your experience matters, and pain is not a requirement for successful breastfeeding. Understanding what’s normal and what isn’t is the first step toward feeding with more comfort and confidence.
Also read: Everything You Need to Know About Ameda Pumps
Knowing what’s normal sets the stage for identifying the specific causes behind ongoing discomfort.
5 Common Reasons Breastfeeding Hurts and How to Fix Them

Breastfeeding hurts for different reasons, and it’s rarely caused by just “one thing.” Sometimes it’s about how your baby is latching, other times it’s related to changes in your body, milk flow, or even the tools you’re using. The key is knowing that pain usually has a specific cause, and once you understand what’s behind it, relief becomes much more achievable.
Below are the most common reasons breastfeeding can feel uncomfortable or painful.
1. Incorrect Latch Or Positioning
An incorrect latch or positioning means your baby isn’t attached deeply or aligned properly at the breast.
A poor latch often feels sharp, pinchy, or toe-curling, especially right when your baby attaches. Instead of a deep pull, it can feel like your nipple is being tugged or squeezed. You might notice that feeding feels harder than it should, even though your baby seems eager.
Here are a few signs worth checking:
- Your baby’s mouth isn’t wide open before latching
- You see more nipple than areola in their mouth
- Their jaw movement looks shallow or choppy instead of slow and rhythmic
- Your nipple looks flattened, creased, or misshapen after a feed
If any of this sounds familiar, it doesn’t mean you’re doing something wrong; it simply means your latch may need a small adjustment.
2. Nipple Trauma, Cracks, And Blisters
When your nipples are sore, cracked, or blistered, it’s usually a sign that they’re taking more pressure than they should. This kind of trauma often builds up quietly, a slightly off latch, frequent feeds without enough healing time, or constant friction can irritate the skin faster than it can recover. Nipples are sensitive, and they don’t need much strain to protest.
You might notice:
- Fine cracks or splits that sting during or after feeds
- Small blisters or shiny, swollen spots on the nipple
- Scabbing or light bleeding that makes feeds feel intimidating
If you find yourself wincing before your baby even latches, that’s your cue to pause and reassess. Nipple damage isn’t something you have to “push through,” and spotting it early can make healing much easier and feeding far more comfortable.
3. Engorgement And Fullness
Engorgement happens when your breasts become overly full, tight, and swollen. When this pressure builds up, the skin stretches, milk flow slows, and feeding can suddenly feel uncomfortable or even painful.
This usually shows up early postpartum, often when your milk first comes in or when feeds are delayed. You may notice:
- Breasts that feel hard, heavy, or warm to the touch
- Skin that looks shiny or feels stretched
- A feeling of pressure that makes latching more difficult for your baby
Engorgement can feel overwhelming, especially when it comes on quickly. The good news is that it’s usually temporary, and with the right support, that tight, painful feeling can ease much faster than you might expect.
4. Yeast Or Bacterial Infections (Thrush)
This kind of pain often feels different, and that’s an important clue. Instead of surface soreness or tenderness, thrush-related pain is usually burning, shooting, or deep, and it can linger even after a feeding ends. Your nipples may look mostly normal, which makes this especially confusing, because the pain feels much bigger than what you can see.
Some common signs to watch for:
- A burning or stinging sensation during and between feeds
- Nipples that appear unusually pink, shiny, or irritated
- Sudden pain after feeding had started to feel comfortable
- In babies: white patches in the mouth, diaper rash that doesn’t clear easily, or fussiness at the breast
Because yeast and bacteria can pass back and forth, both you and your baby may need support at the same time. If the pain feels intense, persistent, or out of proportion to what’s visible, it’s worth getting it checked rather than trying to tough it out.
5. Structural Issues In Your Baby (e.g., Tongue-Tie)
Sometimes the discomfort isn’t coming from your body alone. Certain structural differences in your baby’s mouth, like tongue-tie (a tight piece of tissue under a baby’s tongue), can make it harder for them to move their tongue freely.
When that movement is restricted, your baby may struggle to maintain a deep, effective latch, which can lead to ongoing pain for you even when you’re doing everything “right.”
Professionals usually look for signs such as:
- Difficulty staying latched or frequent slipping off
- Clicking sounds while feeding
- Short or tight tongue movement
- Prolonged feeds with little milk transfer
- Slow weight gain despite frequent feeding
These issues aren’t always obvious at first glance, which is why trained providers assess both how your baby’s mouth moves and how feeding feels for you. Identifying structural challenges early can make a big difference in comfort and feeding success.
Once you know the source, the next step is taking practical action to improve latch and reduce pain.
Step-by-Step Adjustments to Improve Latch and Reduce Pain Immediately

Improving latch isn’t about perfection; it’s about helping your baby attach in a way that supports steady milk flow and protects your comfort at the same time. Even subtle adjustments can create noticeable relief and build confidence from one feeding to the next.
Below are practical, supportive ways to refine latch and positioning.
Understanding Good Latch Principles
A comfortable latch starts before your baby’s mouth even opens. Instead of aiming your nipple straight in, think about guiding your baby’s whole body into position so feeding feels more natural and supported.
A strong latch usually includes:
- Your baby’s body is facing yours, not twisted at the neck
- Chin and nose touching or close to your breast
- A wide, open mouth before attachment
- Lips flanged outward, not tucked in
- Slow, steady jaw movement rather than rapid nibbling
When your baby’s body, mouth, and jaw are aligned, feeding tends to feel smoother and less stressful on your nipples. It’s less about force and more about setup; once alignment clicks, comfort often follows.
Struggling to find the most comfortable latch for you and your baby? ICBP partners with The Lactation Network to connect you with board-certified lactation consultants, in-person or virtually, often covered by insurance. Getting professional guidance can make feeds more comfortable and effective.
3 Breastfeeding Positions That Often Help
Sometimes comfort improves not by changing what you’re doing, but how you’re holding your baby. Different positions support different bodies, and finding the right one can ease strain for both of you.
- Cradle hold: Your baby lies across your chest with their head resting in the bend of your arm. This position offers close eye contact and works well once feeding feels more established.
- Football (clutch) hold: Your baby is tucked under your arm at your side, with their body supported along your forearm. This can give you better visibility and control, especially if you need to guide attachment more closely.
- Laid-back breastfeeding: You recline comfortably and let your baby lie tummy-to-tummy on you. Gravity helps support a deeper latch, and many parents find this position especially relaxing and gentle.
There’s no single “best” position; the one that feels calm and supported is the right place to start.
How To Break Suction Safely
If you ever need to unlatch your baby, doing it gently can make a big difference in how your body feels afterward. Sudden pulling away can increase soreness, so think slowly and calmly.
Here’s an easy way to do it:
- Stay relaxed and bring your clean finger close to the corner of your baby’s mouth
- Gently slide your finger between their gums to release the seal
- Wait for the suction to soften before moving your baby away
- Take a breath before repositioning and trying again
This small pause protects sensitive skin and gives you a moment to reset. Visual guides can help too.
Also read: Prenatal Vitamins Explained: Finding the Best Formula with Folic Acid
Now, let us have a look at how to care for sore, cracked, or bleeding nipples.
Simple Daily Steps to Heal Sore or Bleeding Nipples
When your nipples feel raw or tender, gentle care can make a real difference. Think of healing as creating a calm, protected environment for your skin, not doing more, but doing less, thoughtfully.
Here’s what often helps:
- Safe topical care: Medical-grade lanolin or nipple balms designed for breastfeeding can soothe and protect without needing to be washed off. These are widely supported by clinical guidance for intact skin.
- Air-drying between feeds: Letting nipples dry naturally helps reduce moisture buildup, which can slow healing and irritate sensitive skin.
- Simple, gentle cleansing: Clean water is usually enough. Over-washing can strip your skin of its natural oils.
A few things to skip:
- Alcohol wipes or harsh cleansers, they dry and irritate healing tissue
- Frequent scrubbing or rubbing can reopen cracks
- Random home remedies that aren’t meant for breastfeeding skin
If soreness persists or bleeding doesn’t improve, it’s okay to pause and seek extra support. Healing isn’t about toughness; it’s about care.
Beyond nipple care, managing fullness and engorgement can also relieve pain and support successful feeds.
Quick Techniques to Manage Full Breasts and Ease Pain

When your breasts feel uncomfortably full, relief often comes from helping milk move, gently and intentionally. The goal isn’t to empty everything, but to soften enough so feeding feels easier and your body can settle.
Here are supportive ways to ease that pressure:
- Manual expression: Using your hands to release a small amount of milk can soften the breast and make latching more comfortable.
- Warm shower or compress before feeding: Warmth encourages milk flow and can reduce that tight, stretched feeling.
- Gentle massage: Slow, light strokes toward the nipple help milk move without irritating tender tissue.
Pumping may help when fullness makes feeding difficult or when you need a bit more relief between feeds. Even short sessions can take the edge off without overstimulating supply.
Pay attention to your body. If fullness is paired with redness, fever, worsening pain, or symptoms that don’t improve, that discomfort may be moving beyond normal engorgement and deserves extra attention.
Understanding how engorgement differs from more serious conditions like clogged ducts or mastitis helps you respond appropriately.
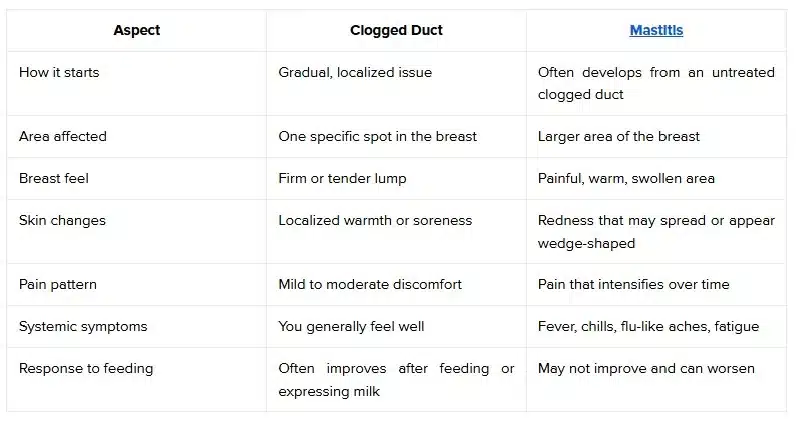
How to Spot Clogged Ducts or Mastitis Before Pain Escalates
Breast pain can escalate quickly if ignored. Recognizing the early signs of clogged ducts versus mastitis helps you respond sooner, reduce discomfort, and prevent minor issues from turning into serious infections.
Below is how these two conditions typically show up and what to look for.
Also read: Breast Pumping Laws in Pennsylvania: Your Rights Explained
Pump-related factors also play a role in comfort, so understanding flange fit and settings is key.
How to Adjust Your Pump and Flanges to Avoid Pain

Pumping should feel supportive, not stressful. When discomfort shows up during pumping, it’s often linked to fit, settings, or worn-out parts rather than milk production itself. Small adjustments in how your pump fits and functions can dramatically change how your body responds.
Below are the most common pump-related factors that influence comfort and how to approach them thoughtfully.
Why Flange Size Matters
Flanges act as the connection point between your body and the pump, so fit truly matters. A good fit allows your nipple to move freely in the tunnel without rubbing or pulling excess skin along with it.
Signs of a better fit include:
- Nipple movement that looks centered and smooth
- Minimal areola is being pulled into the tunnel
- A sensation of gentle pulling rather than pinching
Visual cues of poor fit can include redness, swelling, rubbing, or a feeling that suction is concentrated in one spot instead of evenly distributed.
If your pump isn’t fitting right or causing discomfort, ICBP can help. They handle insurance verification, prescription coordination, and shipping, so you can get a medical-grade breast pump that fits your needs without extra hassle.
Pump Settings And Comfort Tips
Comfort often improves when you let your body set the pace. Starting with lower suction and slowly increasing allows your body to adjust without triggering pain or stress.
A few things to keep in mind:
- Stronger suction doesn’t equal more milk
- Gradual increases are usually more comfortable
- Standard electric pumps provide steady, adjustable suction
- Wearable pumps offer flexibility but may feel different depending on breast shape and movement
Listening to your body’s response is just as important as the pump itself.
Supplies And Replacement Parts That Help Comfort
Sometimes discomfort isn’t about technique; it’s about tired or mismatched parts. Over time, pump components can lose effectiveness, affecting how suction feels.
Supportive supplies include:
- Alternate flange sizes or soft cushions for better comfort
- Clean, properly fitting tubing to maintain smooth suction
- Regularly replace valves and membranes to prevent uneven pressure
Also read: Breast Pumping Laws Michigan: What Moms Should Know
Along with breast pumps, many insurance plans cover essential replacement supplies like valves, membranes, and milk storage bags. ICBP helps you with coverage so you can keep feeding comfortably without worrying about out-of-pocket costs.
Now, let us see some red flags that can indicate the need for professional evaluation.
Warning Signs That Your Breastfeeding Pain Needs Professional Help
Your body is very good at sending signals, and some forms of pain are meant to be listened to, not managed quietly. If discomfort feels intense, constant, or unsettling, it’s okay to pause and reach out for professional support.
Consider seeking evaluation if you notice:
- Pain that doesn’t improve or continues well beyond the early adjustment period
- Sharp or intense pain that happens at every feeding
- Redness that spreads, or symptoms like fever, chills, or feeling unwell
- Your baby is pulling away, refusing feeds, or not gaining weight as expected
Reaching out doesn’t mean you’ve failed; it means you’re protecting both your comfort and your baby’s feeding journey. Getting timely support can prevent small issues from turning into bigger ones.
Accessing professional support is easier when insurance helps cover the right guidance, supplies, and follow-up care.
How Insurance Coverage Can Help You Access Support And Supplies
When you’re already experiencing pain, recovery, and feeding schedules, figuring out insurance shouldn’t feel like another full-time job. Coverage exists specifically to reduce barriers during this stage, not just for equipment, but for guidance and continuity of care that supports long-term feeding comfort. Knowing how insurance helps can change what support feels possible.
Below is how Insurance Covered Breast Pumps (ICBP) helps turn insurance benefits into real, practical support for you:
- Insurance-Covered Breast Pumps: Under the Affordable Care Act, most plans cover medical-grade breast pumps at little or no cost. ICBP works with top brands like Medela, Spectra, Ameda, Lansinoh, Elvie, and Willow, matching you with a pump that fits both your insurance coverage and lifestyle.
- End-to-End Insurance Coordination: ICBP handles benefit verification, prescription (Rx) coordination with your OB/GYN, claim submission, and paperwork, so you don’t have to experience confusing insurance processes on your own.
- Replacement Pump Supplies: Many insurance plans also cover ongoing supplies such as tubing, valves, membranes, flanges, and milk storage bags. ICBP helps you understand what your plan allows and when replacements are eligible.
- Maternity and Postpartum Recovery Products: Depending on your plan, items like maternity support braces, postpartum garments, compression socks, and blood pressure monitors may qualify for coverage, supporting recovery beyond feeding alone.
- Access to Lactation Support: Through a partnership with The Lactation Network, ICBP helps connect you to board-certified lactation consultants (IBCLCs) for in-home, in-office, or virtual visits, often covered by insurance.
By combining insurance expertise with maternal care products and lactation resources, ICBP removes financial and administrative barriers, making it easier for you to focus on healing, feeding comfortably, and caring for your baby.
Conclusion
Pain can influence confidence and overall breastfeeding experience beyond the physical discomfort. The most important takeaway is that pain usually has an explanation, and understanding why it’s happening gives you back a sense of control.
Access to that support shouldn’t depend on guesswork or financial stress. This is where ICBP helps simplify the process by handling insurance verification, coordinating prescriptions, and making it easier to receive covered pumps, supplies, and lactation resources. When logistics are managed for you, it’s easier to focus on healing and feeding comfortably.
Check your insurance eligibility today and see what breastfeeding support and supplies your plan already covers.
FAQs
1. Why does breastfeeding hurt more at night than during the day?
Nighttime feeds can feel more painful due to fatigue, lower pain tolerance, and hormonal shifts that heighten sensitivity. Babies may also latch more urgently when sleepy, which can affect comfort. Quiet surroundings can make discomfort feel more noticeable compared to busy daytime feeds.
2. Can stress or anxiety make breastfeeding pain worse?
Yes. Stress can increase muscle tension and interfere with milk let-down, making feeds feel more uncomfortable. Anxiety may also heighten pain perception. Creating a calm feeding environment and getting reassurance or support can sometimes reduce pain intensity even without physical changes.
3. Is breastfeeding pain different with a newborn versus an older baby?
It can be. Newborn pain often relates to early learning and adjustment, while pain with older babies may be linked to stronger suction, distractions, teething behaviors, or changing feeding patterns. Each stage brings different challenges, so new pain later on is still worth addressing.
4. Why does breastfeeding hurt more on one breast than the other?
Each breast can behave differently. Variations in nipple shape, milk flow, or your baby’s preferred latch can affect comfort. One side may also empty less efficiently, increasing sensitivity. Ongoing one-sided pain deserves attention to rule out underlying issues.
5. Can dehydration cause breastfeeding to hurt?
Dehydration can contribute indirectly by increasing fatigue, slowing recovery, and making tissue feel more sensitive. While it doesn’t directly cause pain, staying well hydrated supports overall comfort and helps your body handle frequent feeding or pumping demands more smoothly.










