Can Breastfeeding Moms Take Ibuprofen? What Research and Doctors Say

If you’re breastfeeding and dealing with pain, whether it’s postpartum soreness, headaches, cramps, or muscle aches, it’s completely natural to pause and ask, “Can I take ibuprofen while breastfeeding?” Wanting relief while also protecting your baby is a careful balance many nursing parents think about.
Clinical studies have shown that ibuprofen passes into breast milk in extremely small amounts, making it a preferred pain-relief option during breastfeeding. Because so little reaches breast milk, healthcare providers commonly recommend it for postpartum pain, headaches, and inflammation.
Still, understanding why it’s considered safe, how to use it properly, and when extra caution is needed can help you feel more confident in your decision. This guide walks you through everything you need to know about ibuprofen use during breastfeeding, so you can manage pain while continuing to care for your baby with peace of mind.
At A Glance
- Ibuprofen is often recommended for postpartum pain, inflammation, headaches, and cramps.
- Standard adult doses are typically safe, and you don’t need to pump and dump.
- It’s best to use ibuprofen short-term and check with a healthcare provider if you need higher doses or long-term relief.
- If your baby was premature or has medical concerns, extra guidance from a pediatrician is recommended.
- Support beyond medication, like proper recovery tools and lactation help, can make breastfeeding easier.
What Is Ibuprofen?
Ibuprofen is a common over-the-counter medication used to relieve pain, reduce inflammation, and lower fever. It belongs to a group of medicines called nonsteroidal anti-inflammatory drugs (NSAIDs), which work by reducing substances in the body that cause pain and swelling.
Ibuprofen is often used for things like:
- Headaches and migraines
- Muscle and joint pain
- Menstrual cramps
- Postpartum soreness
- Inflammation-related pain
- Fever reduction
Is Ibuprofen Safe While Breastfeeding?

Yes, ibuprofen is generally considered safe to use while breastfeeding when taken at recommended doses. It’s one of the most commonly suggested pain relievers for nursing parents because only very small amounts pass into breast milk.
Here’s why ibuprofen is widely viewed as a breastfeeding-friendly option:
- Minimal transfer into breast milk: Only tiny amounts reach breast milk, far below levels known to affect infants.
- Short half-life: Ibuprofen leaves the body relatively quickly, reducing exposure for your baby.
- Commonly used postpartum: It’s often recommended right after birth for pain and inflammation, even while breastfeeding.
- Anti-inflammatory benefits: Helps reduce swelling as well as pain, which can be helpful during recovery.
- No need to pump and dump: When used as directed, you can continue breastfeeding as usual.
As with any medication, if you need high doses for long periods or have specific health conditions, it’s best to check with your healthcare provider.
How Much Ibuprofen Can You Take While Breastfeeding?
For most breastfeeding parents, ibuprofen can be taken in the same doses recommended for adults, unless your healthcare provider advises otherwise. When used correctly, it provides effective pain relief without posing a risk to your baby.
Here’s what to know about dosing and use:
- Typical dose: 400 mg every 4–6 hours as needed
- Prescription doses: May be higher, but should only be taken under medical guidance
- Timing tip: Taking ibuprofen right after breastfeeding or pumping can slightly reduce the already minimal amount that enters breast milk before the next feed
- No pumping interruption needed: You don’t need to pump and dump when taking standard doses
If you find yourself needing ibuprofen frequently or for extended periods, it’s a good idea to talk with your healthcare provider to address the underlying cause of pain and confirm continued safe use while breastfeeding.
Suggested read: Prenatal Vitamins Explained: Finding the Best Formula with Folic Acid
Medications and Breastfeeding: Safety, Timing, and Precautions

When you’re breastfeeding, it’s completely natural to pause before taking any medication, even common over-the-counter ones. While many medications are considered safe, a few thoughtful checks can help you feel more confident about your choices and protect both you and your baby.
Here are key factors to consider before taking medication while breastfeeding:
- How much passes into breast milk: Some medications transfer in very small amounts, while others may pass through more easily.
- Your baby’s age and health: Full-term, healthy babies usually tolerate medications better than premature or medically fragile infants.
- Timing of doses: Taking medication right after a feed can help minimize exposure before the next nursing session.
- Duration of use: Short-term use is often safer than long-term or high-dose use.
- Your own health conditions: Kidney, liver, or stomach issues may affect which medications are appropriate for you.
- Potential side effects: Even rare reactions should be monitored, especially if your baby seems unusually fussy or sleepy.
- Reliable guidance: Trusted sources and healthcare providers can help you understand which medications are compatible with breastfeeding.
When in doubt, reaching out to a healthcare provider or lactation consultant can help you make informed decisions without unnecessary stress.
Ibuprofen vs Other Pain Relievers While Breastfeeding
Not all pain relievers work the same way, and when you’re breastfeeding, safety matters just as much as effectiveness. Some medications pass into breast milk more easily than others, while certain drugs are better suited for short-term use or specific types of pain.
The table below offers a clear comparison to help you understand how ibuprofen stacks up against other commonly used pain relievers during breastfeeding.
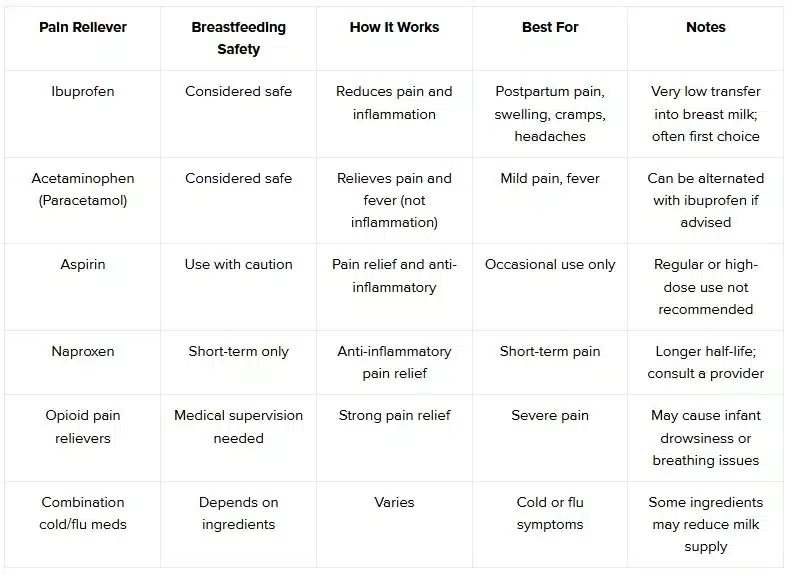
For many breastfeeding parents, this balance makes it a practical and widely recommended option, especially during postpartum recovery.
Suggested read: Breast Pump Supplies Through Insurance
When to Be Cautious With Ibuprofen & Signs to Watch for in Your Baby

While ibuprofen is considered safe for most breastfeeding parents, there are certain situations where extra care or a conversation with your healthcare provider is important. Being informed helps you use it confidently while staying attentive to your baby’s well-being.
You may want to check with a healthcare provider before using ibuprofen if:
- You have a history of stomach ulcers, severe acid reflux, or kidney disease
- You need high doses or long-term pain management
- Your baby was born prematurely or has underlying medical conditions
- Pain feels persistent, severe, or isn’t improving with short-term use
Rare signs to watch for in your baby (these are uncommon but worth noting):
- Unusual fussiness or irritability
- Vomiting or digestive discomfort
- Rash or skin changes
- Changes in feeding patterns or sleepiness
If you notice any of these symptoms or feel unsure at any point, reach out to your pediatrician for guidance. While reactions are rare, staying observant ensures both you and your baby remain safe and supported.
Also Read: Breast Pumping Tips: Finding the Right Pump and Making It Work for You
Supporting Your Recovery While Breastfeeding with ICBP
Pain management is just one part of postpartum recovery. Adequate rest, hydration, nutrition, and the right support tools also matter.
If you’re navigating breastfeeding challenges alongside recovery, Insurance Covered Breast Pumps (ICBP), can help by:
- Verifying insurance coverage for breast pumps and accessories
- Helping you access quality, medical-grade pumps
- Coordinating prescriptions with your healthcare provider
- Connecting families with lactation support when available
Getting the right equipment and guidance can make both recovery and feeding feel more manageable.
Also read: Best Nipple Care Creams for Breastfeeding Moms
Final Thoughts
Managing pain while breastfeeding shouldn’t come with added worry. For most nursing parents, ibuprofen is a safe and effective option when used as directed, offering relief without compromising your baby’s well-being.
If you’re managing breastfeeding challenges alongside recovery, having the right support makes a difference. Insurance Covered Breast Pumps (ICBP) helps families access insurance-covered breast pumps, equipment, and lactation support—so you don’t have to manage it all alone.
Check your insurance eligibility today to explore pump options and breastfeeding resources designed to support you every step of the way.
FAQs
1. Can I take ibuprofen every day while breastfeeding?
Short-term daily use is generally considered safe, but prolonged use should be discussed with your healthcare provider.
2. Do I need to pump and dump after taking ibuprofen?
No. Pumping and dumping is not necessary when taking ibuprofen at recommended doses.
3. Is ibuprofen safe while breastfeeding a newborn?
Yes, for healthy, full-term newborns, ibuprofen is commonly considered safe. If your baby was premature or has health concerns, consult your pediatrician.
4. Can ibuprofen affect milk supply?
Ibuprofen is not known to reduce milk supply when used normally.
5. What’s better while breastfeeding, ibuprofen or acetaminophen?
Both are considered safe. Ibuprofen may be preferred when inflammation is involved, while acetaminophen works well for general pain or fever.










