How to Get a Free Aetna Breast Pump?

If you have Aetna insurance and you’re pregnant, you may be wondering if a breast pump is covered, and how to get one without confusion or stress.
The good news is that many Aetna plans do cover breast pumps at little or no cost. The process can feel unclear at first, but it’s usually straightforward once you know the steps.
This guide walks you through exactly how Aetna breast pump coverage works, what’s typically included, and how to order your pump with confidence.
Key Takeaways
- Many Aetna plans cover breast pumps, often at no cost when you follow plan guidelines.
- Using an in-network supplier matters and helps avoid unexpected expenses.
- Standard electric pumps are usually covered, while wearable or rechargeable models may involve an upgrade fee.
- You do not have to manage the process alone; help is available to make ordering simple.
Get Your Free Aetna Breast Pump in 3 Easy Steps
If you have Aetna insurance, you can often get a breast pump covered at little or no cost by using an in-network provider like Insurance Covered Breast Pumps (ICBP).
Open this link: Order Free Aetna Breast Pump
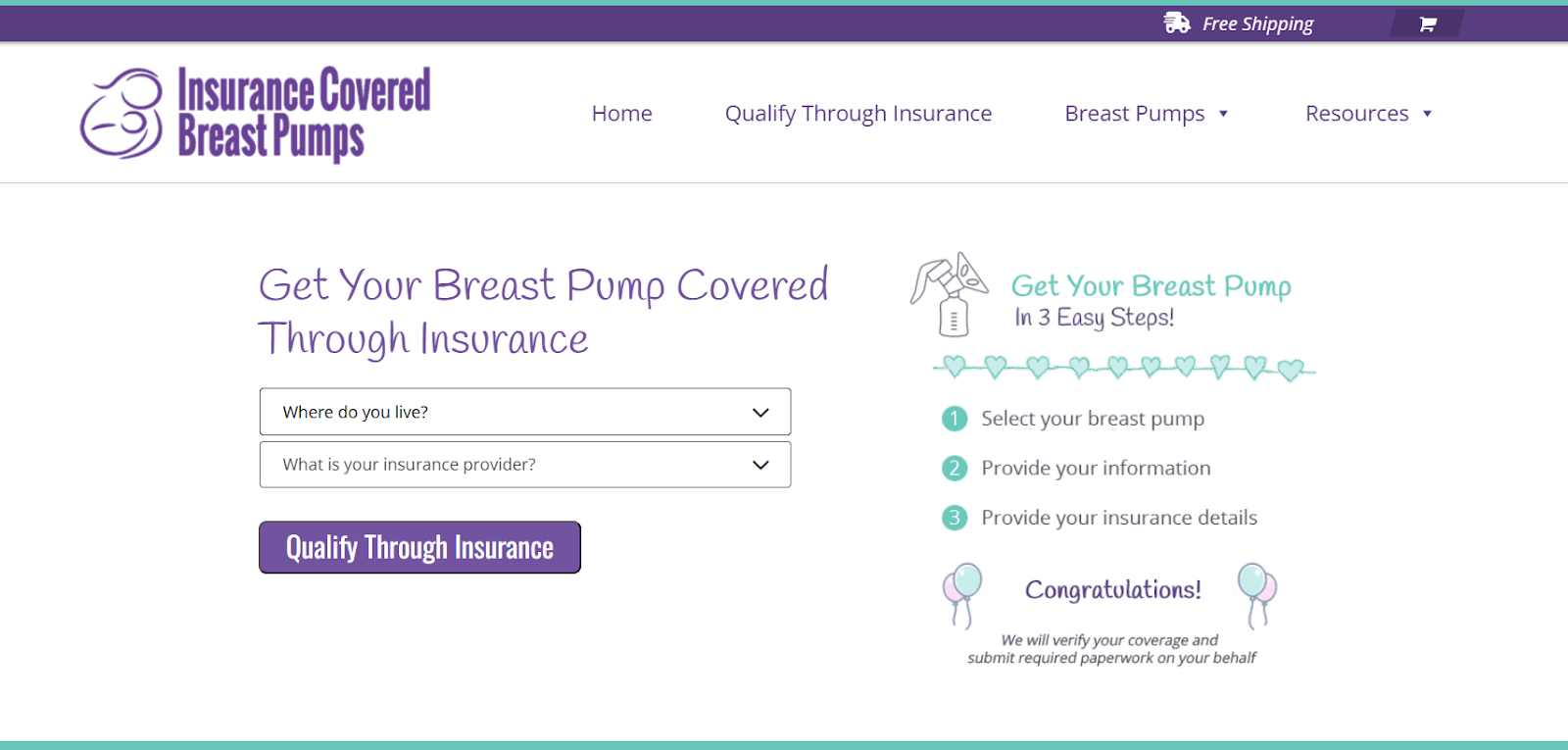
- Select your breast pump: Choose from Aetna-covered options or upgrade if you prefer.
- Provide your information: Enter your basic details so your prescription and delivery can be coordinated.
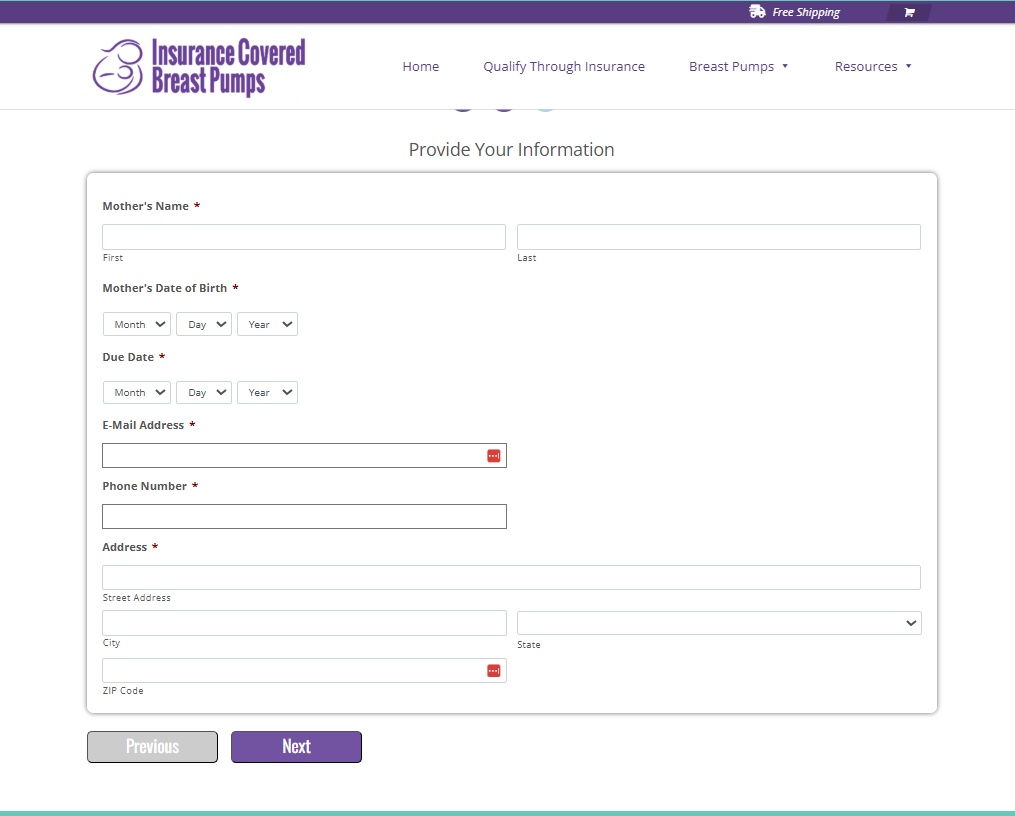
- Add your Aetna insurance details: ICBP verifies your coverage and handles all paperwork for you.
Once submitted, ICBP takes care of the rest. Your breast pump is shipped free, nationwide, directly to your home.
Quick Answer First: Yes, Aetna Often Covers a Breast Pump
In many cases, Aetna does cover a breast pump, and for many moms, that means paying nothing out of pocket. Coverage is part of preventive maternity care under federal guidelines, but the exact details depend on your specific plan.
Here’s what usually determines whether your Aetna breast pump is covered:
- Your plan type (PPO, HMO, EPO, or Medicaid)
- Using an in-network breast pump supplier
- Having a prescription from your healthcare provider
When these pieces are in place, most moms receive a standard electric breast pump through insurance. Some plans also allow upgrades to wearable or rechargeable models for an added fee.
If you’ve heard the phrase “free Aetna breast pump,” it typically means the pump is covered through insurance, not that every model is automatically included. Knowing this upfront helps set clear expectations and avoid surprises.
Why Aetna Covers Breast Pumps in the First Place

Breast pump coverage exists because breastfeeding support is considered an essential part of maternity care. Under the Affordable Care Act, most health insurance plans are required to cover breastfeeding equipment and support.
For Aetna members, this means a breast pump is often treated as durable medical equipment (DME). Instead of buying a pump on your own and asking for reimbursement, coverage usually works best when you order through an approved, in-network supplier.
It’s important to know that not all Aetna plans are identical. Employer-sponsored plans, student health plans, and Medicaid programs may follow slightly different rules. That’s why checking your specific benefits matters, not because coverage is unlikely, but because the process can vary.
Once you understand your plan’s guidelines, the rest of the steps become much easier to follow.
Check Your Aetna Plan in 5 Minutes
Before choosing a pump, it helps to confirm exactly what your Aetna plan covers. This step sounds intimidating, but it’s usually quick and saves time later.
Start by logging into your Aetna member portal or checking your plan documents. Look for sections labeled maternity benefits, preventive care, or durable medical equipment. If things still feel unclear, a short call to member services can give you direct answers.
When speaking with an Aetna representative, you can ask:
- Is a breast pump covered under my plan?
- Do I need a prescription to order one?
- Which breast pump suppliers are in network?
- What breast pump models are fully covered?
- Are replacement parts or supplies included?
Keep notes during the call. Knowing whether your plan is PPO, HMO, or Medicaid-based can also help clarify requirements. Many moms find that once these questions are answered, the rest of the process feels much more manageable.
Also Read: Aetna Insurance Coverage for Willow Breast Pumps
What Types of Breast Pumps Aetna Usually Covers
Most Aetna plans cover one standard electric breast pump as part of maternity care. These pumps are designed for regular daily use and work well for most breastfeeding needs.
Commonly covered options include:
- Manual breast pumps, though these are less common
- Standard double electric breast pumps, which are the most frequently covered
Some plans may also cover a hospital-grade breast pump rental, but this usually requires medical documentation and prior authorization. These rentals are often approved for specific medical situations, such as premature birth or supply challenges.
It’s also helpful to know that coverage often applies to one pump per pregnancy or within a specific time period, depending on your plan. While the exact model may vary by supplier, you’ll usually have several reliable options to choose from.
If you’re hoping for a wearable or rechargeable pump, those are often available as upgrade options for an added cost. Knowing what’s covered versus upgraded helps you choose what fits your lifestyle without surprises.
When to Order Your Aetna Breast Pump

Timing can feel confusing, but ordering your Aetna breast pump is usually more flexible than many moms expect. Most plans allow you to place your order during pregnancy or shortly after delivery.
Many moms choose to order in the third trimester. Doing so gives enough time for insurance approval, prescription coordination, and shipping. It also means your pump is ready when your baby arrives, instead of scrambling afterward.
If you’ve already delivered, don’t worry. Many Aetna plans still allow you to order your pump postpartum. The key is checking your plan’s specific rules and acting as soon as you can.
Ordering earlier often feels easier because:
- Your healthcare provider is already involved in prenatal care
- There’s less urgency if the paperwork takes a few days
- You can compare pump options without pressure
Once timing is clear, the next step is usually simpler than expected.
The Prescription Step (It’s Usually Simple)
Most Aetna plans require a prescription for a breast pump, but this step is often quick and routine. Your OB-GYN, midwife, nurse practitioner, or primary care provider can write it.
In many cases, the prescription only needs to state that a breast pump is medically necessary for postpartum use. You don’t usually need a special diagnosis or extra documentation.
Many in-network suppliers, including Insurance Covered Breast Pumps (ICBP), can help coordinate this step for you. They’ll contact your provider directly and make sure the prescription meets Aetna’s requirements.
If you’re requesting a hospital-grade rental or special supplies, additional approval may be needed. For standard electric pumps, the prescription process is usually straightforward and stress-free.
Once the prescription is on file, you’re ready to choose a supplier and move forward with ordering your pump.
Also Read: Pregnancy Freebies Every Mama Should Know About (and How to Get Them)
Use an In-Network Breast Pump Supplier to Maximize Coverage

This step is one of the most important — and most commonly missed. To get the most coverage from Aetna, you’ll usually need to order your breast pump through an in-network durable medical equipment (DME) supplier.
Using an in-network supplier helps ensure:
- Your pump is billed correctly to insurance
- You avoid unexpected out-of-pocket costs
- Claims are handled on your behalf
Aetna maintains a list of approved breast pumps and DME providers, but finding and contacting the right one can feel overwhelming. That’s where a full-service provider like Insurance Covered Breast Pumps (ICBP) can help. ICBP verifies your benefits, confirms network status, coordinates your prescription, and submits claims directly to Aetna.
If you order from an out-of-network supplier, coverage may be reduced or denied entirely. Before placing an order, always confirm that the supplier works directly with Aetna and understands breast pump billing.
Choosing the right supplier often makes the difference between a smooth experience and weeks of back-and-forth.
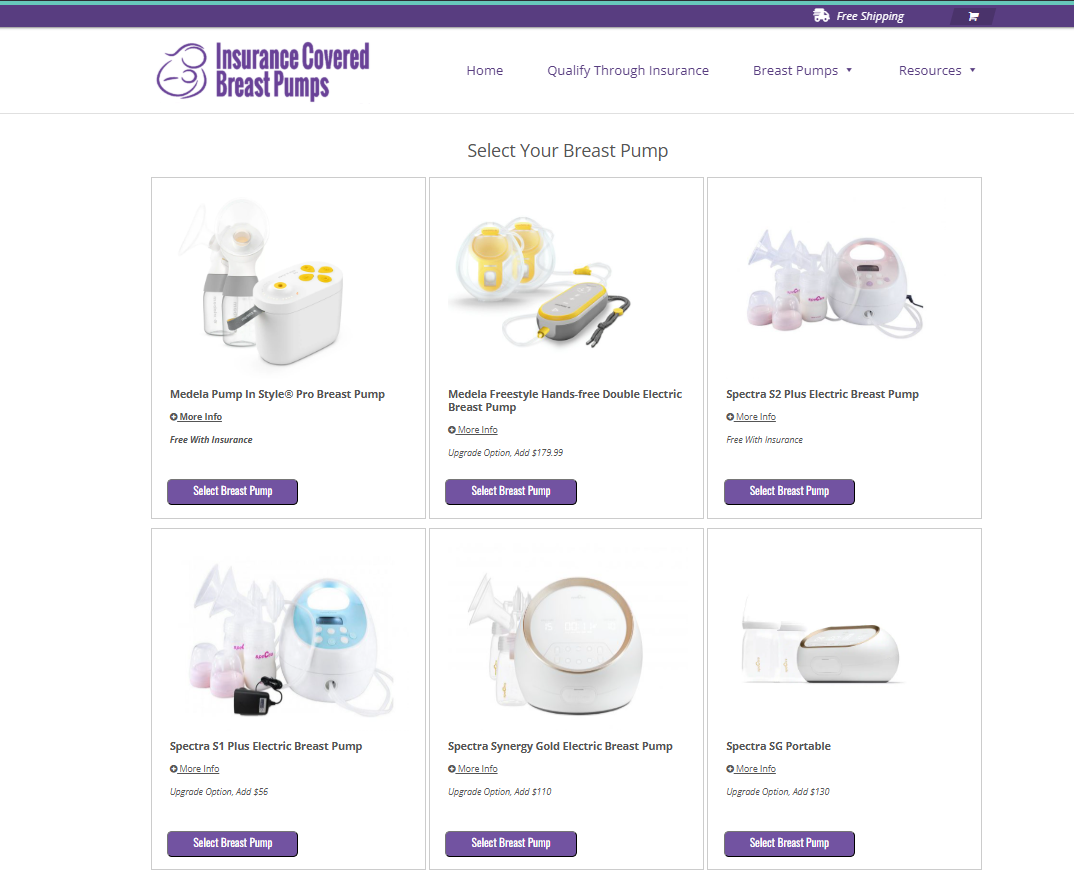
Breast Pump Brands Covered by Aetna: What to Expect
Aetna doesn’t publish a universal list of covered breast pump brands. Instead, available options depend on your plan and the supplier you use. Most moms are offered a selection of reliable, standard electric breast pumps that meet insurance guidelines.
Common brands you may see include:
- Spectra
- Medela
- Lansinoh
- Motif
Some models, like the Spectra S2, are often fully covered. Others, such as rechargeable or wearable pumps, may be available as upgrade options for an added cost.
For example, pumps like Elvie or Willow are sometimes offered with an upgrade fee rather than full coverage.
Your supplier can explain which pumps are covered at no cost and which require an upgrade. Asking upfront helps you choose a pump that fits your routine and budget without surprises.
Also Read: Spectra S2 vs S9: Choosing the Best Breast Pump
Covered vs. Upgrade Pumps: What That Really Means
When ordering a breast pump through Aetna, you’ll likely see two categories: covered pumps and upgrade options. Understanding the difference helps you decide without confusion.
A covered pump is usually a standard double electric model that meets Aetna’s requirements. These pumps are reliable, effective, and often come at no out-of-pocket cost when you use an in-network supplier.
An upgrade pump offers additional features, such as:
- Rechargeable batteries
- Quieter motors
- Wearable or hands-free designs
If you choose an upgrade, Aetna typically covers the cost of the standard pump, and you pay the price difference. The supplier sets this fee and varies it by model.
Many moms choose an upgrade because it fits their lifestyle better, especially if they plan to pump at work or on the go. Others prefer a fully covered option to keep things simple. There’s no right or wrong choice; it’s about what works best for you.
Supplies, Replacement Parts, and Other Coverage Limits

In addition to the pump itself, some Aetna plans also cover breast pump supplies, though coverage varies. These may include:
- Replacement valves or membranes
- Tubing
- Flanges
Supplies are often covered on a schedule, such as every few months, and usually require a prescription on file. Your supplier can help track eligibility and reorder items when the time is right.
It’s important to know that storage bags, extra bottles, or accessories may not always be included. Hospital-grade pump rentals and replacement parts beyond basic supplies may also require special approval.
Checking these details early helps you plan and avoid last-minute stress, especially during those busy first weeks after birth.
Extra Aetna Breastfeeding Benefits You Might Not Know About
Your Aetna benefits may include more than just a breast pump. Many plans also offer breastfeeding support services, which can be especially helpful in the early weeks.
Some Aetna plans cover:
- Lactation consultations, either in person or through telehealth
- Breastfeeding education and support programs
- Guidance for pumping challenges, latch concerns, or supply questions
Coverage depends on your plan type, but these services are often considered preventive care. If you’re unsure what’s included, your Aetna representative can confirm what breastfeeding support is available.
For moms ordering through Insurance Covered Breast Pumps (ICBP), there’s also access to lactation support through their partnership with The Lactation Network, when eligible. This can make it easier to get expert help without extra paperwork.
These added benefits exist to support you, not overwhelm you. Even one conversation with a lactation professional can bring reassurance during a time when questions feel endless.
Conclusion
Preparing for a baby comes with enough decisions. Getting a breast pump through Aetna should not feel like another hurdle. For many moms, coverage is available, and the process becomes manageable once you understand the steps.
By checking your plan, using an in-network supplier, and having a prescription ready, you can often receive a breast pump with little or no cost. Knowing the difference between covered and upgrade options also helps you choose what fits your lifestyle without surprises.
If navigating insurance feels overwhelming, support is available. Insurance Covered Breast Pumps (ICBP) helps verify coverage, coordinate prescriptions, and handle paperwork so you can focus on what matters most, caring for yourself and your baby with confidence.
FAQs
1. Does Aetna cover breast pumps?
Yes. Many Aetna plans cover a breast pump as part of maternity care, though coverage details vary by plan.
2. How do I order a breast pump through Aetna?
Check your benefits, choose an in-network supplier, get a prescription, and place your order through the supplier.
3. Which breast pumps are covered by Aetna?
Most plans cover a standard electric breast pump. Available brands and models depend on your plan and supplier.
4. Does Aetna cover breast pump supplies?
Some plans cover replacement parts like valves or tubing on a schedule. Coverage varies, so confirm with your supplier.
5. Does Aetna cover hospital-grade breast pump rentals?
Hospital-grade rentals may be covered with medical need and prior authorization. This depends on your specific plan.










