Aetna Insurance Coverage for Willow Breast Pumps

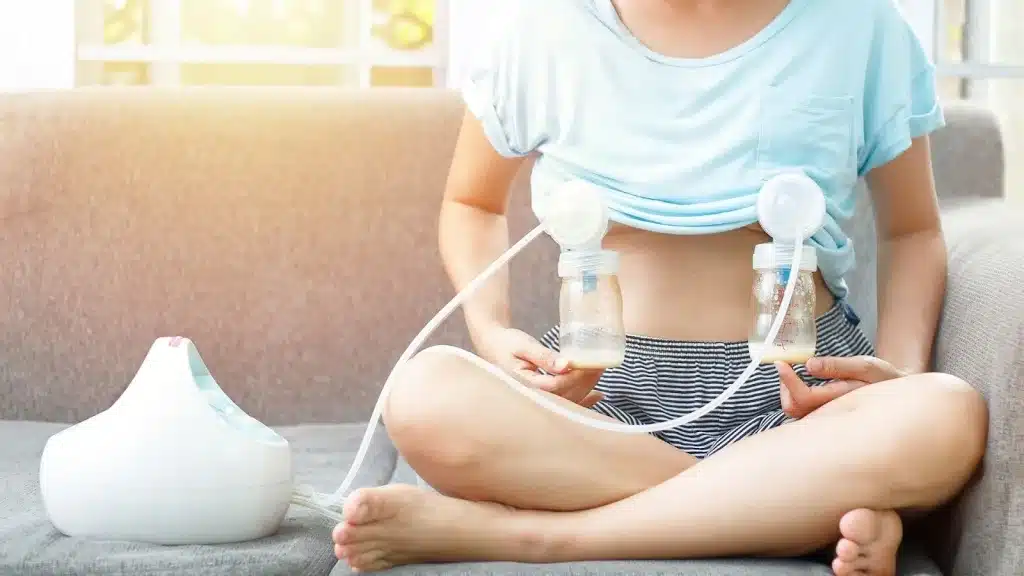
When you’re preparing for your breastfeeding journey, having the right breast pump can make all the difference. For many moms, the Willow wearable pump is appealing because of its quiet, hands-free design that lets you pump while caring for your baby, or even while working. But before investing, it’s important to understand what your Aetna insurance plan covers.
Under the Affordable Care Act (ACA), most insurance providers, including Aetna, are required to cover the cost of a breast pump. The details, like which pumps are included and whether you need a prescription, can vary depending on your individual plan and state regulations.
At a Glance:
- Aetna covers breast pumps under ACA requirements, but the type (manual, electric, wearable) depends on your plan.
- Willow may not be fully covered, but many moms can apply their benefit toward it and just pay the difference.
- Pump bags and supplies (like storage bags or replacement parts) may also be covered when ordered through in-network suppliers.
- Lactation support is often included, giving you access to consultants for added help.
- Best step: Call Aetna and confirm what your plan allows before placing an order.
Types of Breast Pumps Covered by Aetna
When it comes to breast pumps, Aetna’s coverage can look a little different depending on your plan, but in general, most moms can expect some type of support. Let’s break it down in simple terms:
- Manual pumps: These are the small, hand-operated pumps. They’re light, quiet, and great for occasional use or travel. Aetna almost always covers these, though many moms prefer electric options for daily pumping.
- Standard electric pumps: This is the most commonly covered category. These pumps plug in (some also have batteries) and are designed for everyday use. They offer steady suction and efficiency, making them a popular choice for moms who pump at work or need a reliable routine.
- Hospital-grade pumps: Some Aetna plans also provide coverage for hospital-grade pumps, especially if your doctor recommends one. These pumps are stronger and often suggested for moms who are exclusively pumping, working on boosting supply, or have babies in the NICU.
- Wearable pumps, like Willow: This is where coverage can vary. Because Willow is a premium, hands-free wearable pump, it may not be fully covered under every plan. Some moms find that Aetna covers a “basic electric pump” cost, and then they can upgrade to Willow by paying the difference. Others are lucky enough to have it fully included. The key is checking your exact plan to know what’s possible.
How to Verify Your Coverage?

Insurance language can feel overwhelming, but checking whether Aetna covers the Willow pump doesn’t have to be stressful. Think of it as three simple steps to get clarity before you order:
- Look at your policy documents: Start by checking your Aetna plan’s maternity or breastfeeding benefits section. Many moms find this information in their member portal or welcome packet. It should outline whether breast pumps are included and if specific brands, like Willow, are mentioned.
- Call Aetna directly: A quick call can save you a lot of guesswork. Ask them:
-
-
- “Does my plan cover the Willow breast pump?”
- “If not, can I apply my benefit toward an upgrade?”
- “Do I need a prescription or prior approval?”
Jot down the representative’s name and reference number—this can be handy if there’s ever confusion later.
- “Does my plan cover the Willow breast pump?”
-
- Double-check requirements: Some Aetna plans may ask for a doctor’s prescription or a pre-authorization before approving your pump. Don’t worry, most providers are used to this and can get it done quickly during a routine prenatal visit.
Pro tip: If you’re close to your due date, don’t wait until baby arrives to sort this out. Calling a few weeks ahead means you’ll have your pump ready when you need it most.
Steps to Get Your Willow Breast Pump Covered

Once you’ve confirmed that Aetna will cover all or part of your Willow pump, the next step is actually getting it in your hands. Here’s a smooth path to follow:
- Talk with your healthcare provider: If your plan requires a prescription, ask your OB-GYN, midwife, or family doctor. Most providers are used to this request and can give you the prescription during a routine visit.
- Choose an in-network supplier: Aetna works with specific breast pump suppliers like Aeroflow or Insurance Covered Breast Pumps. Ordering through an approved supplier ensures your claim gets processed correctly, and it saves you the headache of chasing reimbursements later.
- Submit your paperwork: Depending on your plan, you may need to provide:
-
-
- Your doctor’s prescription (if required)
- Proof of coverage or a pre-authorization form
- An itemized receipt if you’ve already purchased your pump
- Your doctor’s prescription (if required)
-
- Many suppliers will handle this step for you, which means less stress and faster approval.
Pro tip: If you’re leaning toward Willow but your plan only covers a basic pump, ask the supplier if you can apply your benefit toward an upgrade. Lots of moms are surprised to learn this is an option!
Getting the Most Out of Your Aetna Breastfeeding Benefits

Breastfeeding benefits from Aetna aren’t limited to just getting a pump. Many moms don’t realize their plan may also include tools, services, and upgrades that can make feeding more comfortable and less stressful. Here’s how to make the most of what’s available.
What You Might Have Access To:
- Lactation consultations: Some Aetna plans cover sessions with certified lactation consultants, either in person or virtually. This can be a game-changer if you’re experiencing challenges like latching issues, low supply, or discomfort.
- Replacement parts and accessories: Over time, parts like valves and membranes wear out and affect your pump’s performance. Many plans cover replacements, which helps maintain strong suction without extra cost.
- Milk storage and cleaning supplies: Items like breast milk storage bags, bottles, sterilizing bags, and cleaning wipes may be included. These little things add up quickly, so having coverage helps stretch your budget.
- Upgrades to premium pumps: If your plan only covers a standard pump, you can often apply that benefit toward a premium pump like Willow. You’d just cover the difference, giving you access to hands-free convenience at a lower personal cost.
- Postpartum support services: In addition to breastfeeding supplies, some Aetna plans also include coverage for postpartum counseling or support programs. This holistic care can make a big difference in your recovery and overall well-being.
Tips to Maximize Your Benefits:
- Ask early: Don’t wait until after delivery, call Aetna or your supplier in your third trimester so your pump is ready when you need it.
- Keep receipts: Even if an item seems covered, having receipts makes reimbursements smoother and avoids delays.
- Check annually: Some plans allow for pump part replacements or supplies once a year, so you may be able to refresh your kit as needed.
- Use in-network suppliers: Ordering through Aetna’s approved partners makes the process simpler and increases the chance of full coverage.
- Ask directly about Willow: Even if Willow isn’t listed online, customer service reps can confirm if your plan allows upgrades.
Final Words
Managing insurance coverage for breast pumps and even handy extras like pump bags can feel overwhelming at first. But with the right information, you’ll find that it doesn’t have to be complicated. Aetna, along with providers like Insurance Covered Breast Pumps, makes it possible to access the tools you need to feel confident and supported in your breastfeeding journey.
If you choose a standard pump or upgrade to something more advanced like Willow, remember this: the right pump is the one that works for you. Pairing it with the right accessories, like a reliable pump bag, can make everyday pumping simpler, more organized, and less stressful.
At the end of the day, what matters most is that you feel equipped and supported as you care for your baby. You deserve convenience, comfort, and peace of mind, because feeding your little one should be about bonding, not barriers.
FAQs
-
Does Aetna cover the Willow breast pump?
Coverage varies. Some Aetna plans fully cover Willow, while others only cover a standard electric pump. In many cases, you can use your benefit for a basic pump and pay the difference to upgrade to Willow.
-
Do I need a prescription to get a breast pump through Aetna?
Some plans require a prescription from your OB-GYN or healthcare provider, while others don’t. It’s always a good idea to check early so you’re ready before baby arrives.
-
Are breast pump bags covered by insurance?
Yes, in many cases. Through suppliers like Insurance Covered Breast Pumps, you may be able to get a pump bag covered under your plan. These bags are designed to fit pumps like Spectra, Medela, or Willow and make daily pumping more organized.
-
Can I order my pump and bag before my baby is born?
Yes! In fact, it’s recommended to order during your third trimester. That way, your pump and bag are ready to use as soon as your baby arrives.
-
What if my plan doesn’t fully cover Willow?
You still have options. Many suppliers let you apply your coverage amount to Willow and simply pay the difference out of pocket.
-
Besides the pump and bag, what else might Aetna cover?
Some plans also cover replacement pump parts, milk storage bags, sterilizing supplies, and even lactation consultations. Ask your insurance rep or supplier to see the full list.










