Does the Hospital Give You a Breast Pump? What to Expect After Delivery

If you are wondering whether the hospital gives you a breast pump, you are probably trying to understand what feeding support will look like after delivery. That is such a normal thing to think about, especially when everything else already feels like a lot. Between doctor visits, baby prep, and trying to rest, the last thing you need is confusion about something this important. You deserve clear answers that help you feel more prepared, not more overwhelmed.
Many moms searching ‘does the hospital give you a breast pump?’ are really hoping to avoid surprises once they are recovering and caring for a newborn. You want to know what the hospital helps with, what you will need at home, and how insurance fits into all of it. Having that clarity ahead of time can bring real peace of mind during an emotional, exhausting season.
Key Takeaways
- Hospitals provide clinical-grade pumps mainly when feeding challenges or medical conditions prevent direct breastfeeding in the early days.
- Access typically continues while specific medical or feeding goals are being monitored, not automatically through discharge.
- Hospital pumps focus on early milk production support, while personal pumps are designed for ongoing daily use after you return home.
- Milk collection, labeling, fortification, and timing are closely coordinated with NICU care plans to support fragile babies.
- Most ACA-compliant plans include a personal breast pump benefit, but ordering rules, suppliers, and documentation requirements vary.
When Do Hospitals Provide a Breast Pump to New Moms?
Sometimes, pumping support is not optional; it is part of your baby’s care plan. Hospitals step in when direct nursing is not possible or not effective yet, and timing really matters in those first hours and days.
Common medical situations when staff bring in a pump include:
- Postpartum Recovery Delays: After a C-section, hemorrhage, or magnesium treatment, pumping protects milk supply when early skin-to-skin or latching is postponed.
- Infant Glucose Stabilization: If the baby needs monitored feeds for low blood sugar, pumping helps collect colostrum for syringe or supplemental feeding protocols.
- Respiratory Support Needs: Babies on CPAP or oxygen often cannot coordinate suck-swallow-breathe, so pumping makes sure breast milk is available for tube or bottle feeds.
- Oral Function Challenges: Tongue-tie, cleft palate, or weak suck may require expressed milk while feeding specialists assess and support latch development.
- Maternal-Infant Infection Precautions: Temporary separation for infection control can require pumping to maintain supply until direct breastfeeding is cleared.
If any of these come up, you are not behind; you are adapting. Early pumping in these moments helps protect both your supply and your baby’s access to your milk.
5 Types of Breast Pumps Typically Provided By Hospitals

When a hospital brings you a pump, it is not the kind you toss in a diaper bag. These are clinical machines designed to protect milk supply during medical or feeding challenges.
Hospital-provided pumps differ in several important ways and are set up specifically for short-term medical use:
- Hospital-Grade Double Electric Pump (In-Room Use): This is the large plug-in pump brought to your bedside after birth. It is designed to stimulate milk production in the early days, especially if the baby is sleepy, premature, or having trouble latching.
- NICU Pumping Stations: If your baby is in the NICU, you will likely pump at a bedside station or in a lactation room. The motor is shared, but you receive your own sterile kit that is used only for you.
- Postpartum Recovery Pump: Some moms use a hospital pump during recovery even if the baby is rooming in. It may be recommended if the baby has blood sugar concerns, jaundice, weight loss, or latch difficulties.
- Lactation Consultant Teaching Pump: During a lactation visit, a consultant may use a hospital pump to check flange fit, observe milk flow, and help you practice comfortable positioning and technique.
- Hospital Pump Rental Units: Many hospitals offer rental programs for the same hospital-grade pumps used in your room. These are often recommended if your baby is premature or if you need extra support building supplies at home.
These pumps are built for medical-grade milk stimulation, not everyday portability. They give your body strong early signals while your feeding routine is still being established.
If you want to better understand how pumping supports feeding flexibility, read next: The Importance Of A Breast Pump
How Long Can You Use a Hospital Breast Pump?

The timeline depends on your baby’s medical plan and your milk supply response. Hospital access is tied to clinical milestones, while rentals follow documented need.
Care teams look at several factors to decide duration and when transitions happen:
- Inpatient Care Window: Pump access continues throughout admission, documented in your chart, with session frequency often set at 8–10 expressions per 24 hours.
- NICU Feeding Milestones: Use continues until the baby demonstrates coordinated suck–swallow–breathe or reaches oral feeding targets set by neonatology and speech therapy.
- Milk Volume Benchmarks: Lactation teams track daily output trends; sustained volumes near infant needs can trigger transition planning to a personal pump.
- Post-Discharge Rental Orders: Providers write time-limited rental scripts, commonly 30-day intervals, renewed based on weight gain, transfer volumes, or exclusive pumping status.
- Follow-Up Reassessment Visits: Outpatient lactation visits reassess flange fit, output, and infant transfer; improved direct feeds may support weaning off the hospital-grade unit.
You are not expected to guess when to switch. Your care team uses feeding data and your comfort to guide the timing safely.
The Difference Between a Hospital Pump and a Personal Breast Pump
Both pumps remove milk, but they are engineered for very different stages and settings. One supports clinical feeding plans; the other fits daily life once you are home.
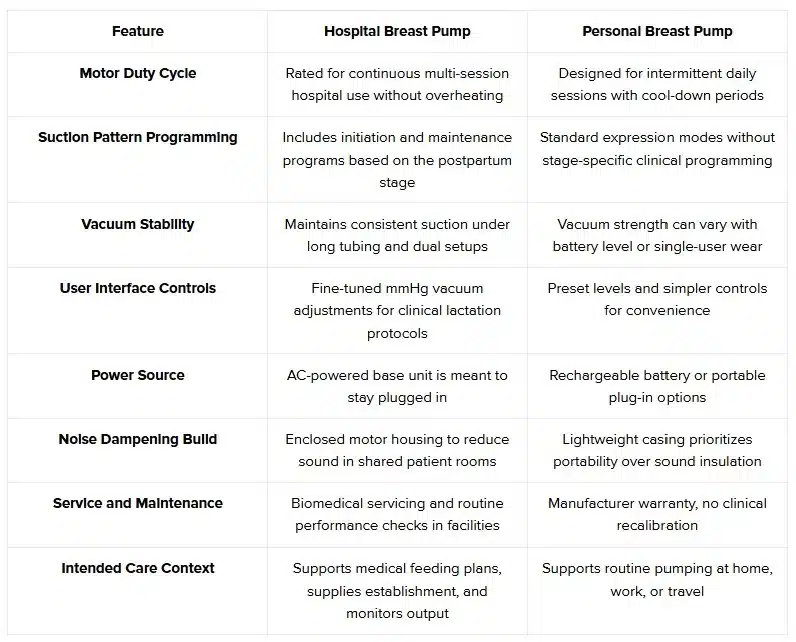
Both pumps support your feeding goals; they simply serve different phases of the journey. One is built for medical intensity, the other for everyday motherhood.
If you’re still deciding which pump fits your routine best, this guide can help: How to Choose the Right Breast Pump For You
What Happens After You Leave the Hospital?

Going home is a big shift. Your feeding plan moves from bedside support to a home routine, and a few practical steps keep milk production steady.
Here is what care teams expect you to set up once you are discharged:
- Milk Transport Plan: Frozen hospital milk is released with proper labeling; bring an insulated cooler with frozen gel packs to keep it at a safe temperature.
- Home Pump Setup: Assemble your personal pump, confirm flange sizing from discharge notes, and record baseline output to share at your first pediatric follow-up.
- Feeding Method Alignment: Follow the written plan, paced bottle, tube, or direct nursing trials, based on infant stamina, transfer volumes, and weight gain targets.
- Storage Rotation System: Date and time every container; use a first-in, first-out method, and separate NICU milk if fortification or special handling is required.
- Outpatient Lactation Follow-Up: Schedule a weighted feed within 3–5 days; consultants compare pre/post weights to adjust pumping frequency or flange fit.
You are building a rhythm now, not starting from scratch. A clear home setup makes those early weeks feel much more manageable.
Special Situations: Pumping While Baby Is in the NICU

When your baby is in the NICU, pumping becomes part of their medical care plan. Your milk supports growth, gut protection, and immune support while feeding skills are still developing.
NICU-specific pumping practices care teams often guide parents through include:
- Colostrum Collection Protocols: Early drops are drawn into sterile oral syringes, labeled for bedside use in mouth care to deliver immune factors before full feeds begin.
- Fortification Planning: Your milk may be combined with a human milk fortifier to meet higher-calorie and protein needs to meet preterm growth targets.
- Timed Pumping Around Rounds: Many units coordinate pumping before medical rounds so fresh milk is available for the next scheduled gavage or bottle feed.
- Milk Handling Verification: Barcoded labels and double-check systems confirm milk matches your baby before storage, thawing, or feeding in the NICU.
- Kangaroo Care Pumping Boost: Pumping immediately after skin-to-skin sessions often improves output due to oxytocin release and improved milk ejection.
This phase can feel overwhelming, but every drop truly matters here. Your NICU team helps turn pumping into powerful medicine for your baby.
Does Insurance Cover a Breast Pump for Home Use?
Yes, in most cases it does. Under U.S. law, breast pumps are considered preventive maternal care, which means many plans must include this benefit.
Here’s how insurance coverage for home pumps typically works:
- Preventive Care Mandate: ACA-compliant plans must include breastfeeding support and equipment, which often covers one personal-use pump per pregnancy.
- In-Network Supplier Rules: Many insurers require ordering through approved durable medical equipment (DME) suppliers rather than buying in-store and submitting receipts.
- Prescription Requirements: Some plans require a provider-issued prescription that lists medical necessity, pump type, or an estimated due date before shipment is approved.
- Upgrade Fee Structures: If you choose a premium wearable or specialty model, insurance may cover the base cost while you pay the price difference.
- Replacement Parts Coverage: Some insurance plans may cover certain pump supplies, such as tubing, valves, flanges, or milk storage bags. Coverage details and replacement frequency vary by plan.
Coverage details can feel confusing, but you usually qualify for more support than you think. Getting help with verification makes the process much easier.
How to Get an Insurance-Covered Breast Pump Without the Stress
Getting a pump through insurance can feel confusing, especially late in pregnancy or right after birth. Breaking it into clear steps makes it much more manageable.
Here’s how most moms successfully move through the process:
- Verify Coverage Details: Call the member services number on your card and ask about breast pump benefits, covered types, and whether a prescription is required.
- Confirm Approved Suppliers: Insurance plans often require you to order through specific in-network medical equipment providers, not general retail stores.
- Request Provider Documentation: If needed, ask your OB or midwife for a prescription that includes your due date and specifies an electric breast pump.
- Choose Pump Within Plan Rules: Review which models are fully covered versus upgraded options that may include an additional out-of-pocket fee.
- Track Order And Delivery Timing: Once approved, confirm shipping timelines so your pump arrives before delivery or soon after returning home.
Taking it step by step prevents last-minute stress. A little planning now makes feeding logistics much smoother once the baby arrives. You can check your insurance options and see what breast pump coverage may be available to you. Get in touch with us!
Final Thoughts
You are stepping into a season where flexibility matters more than perfection. Some days will feel smooth, others might feel uncertain, and both are completely normal. The small choices you make now can quietly remove pressure later, giving you more room to rest and adjust. Trust yourself to take things one day at a time, not all at once.
As everything shifts after the baby arrives, your confidence will grow right alongside your routine. Support looks different for everyone, and finding what works for you is part of the process. There is no single “right” path, only the one that fits your family best. You have more strength and instinct than you realize.
If checking one more thing off your list would bring peace of mind, you can take a minute to see whether you qualify for an insurance-covered breast pump and understand your options before baby arrives.
FAQs
1. Does the hospital give you a breast pump after delivery?
Most hospitals provide access to a pump during your stay if there is a feeding or medical need, but they usually do not send one home with you.
2. Does the hospital provide breast pump support if the baby cannot latch?
Yes, if your baby has trouble latching or feeding effectively, staff often bring in a pump to help protect your milk supply while feeding plans are adjusted.
3. Do hospitals provide breast pumps for every mom automatically?
Not automatically. Pump use is typically based on feeding challenges, separation, or medical situations rather than being routine for all births.
4. Will the hospital provide a breast pump if my baby is in the NICU?
Yes, NICU moms are usually set up with a hospital pump quickly so milk can be expressed and given to the baby even before direct breastfeeding begins.
5. Do hospitals give you a breast pump to keep when you leave?
In most cases, no. The pumps used in the hospital stay there, so moms usually arrange a personal pump for home through insurance or rental.










