Postpartum Preeclampsia: Symptoms, Causes, and Treatment

You’ve done something extraordinary, brought a life into the world. Amidst the joy, exhaustion, and constant adjustments of postpartum life, it’s easy to assume the hardest part is over. The pregnancy is behind you, the baby is here, and now it’s all about healing and bonding, right?
But sometimes, even after birth, your body might still be dealing with hidden challenges. One of these is something many mothers haven’t even heard of: postpartum preeclampsia.
This condition can appear days or even weeks after delivery, sometimes in women who had no signs of high blood pressure during pregnancy. That’s why having even a simple understanding is so important.
Not to scare you, but to empower you. Because healing doesn’t stop at delivery, and neither does your strength.
Here’s what this guide will help you with:
- Understand postpartum preeclampsia, even if you had no signs during pregnancy.
- Identify key symptoms, such as severe headaches, vision changes, or sudden swelling.
- Learn how it’s diagnosed and treated, including common tests and medications.
- Take simple steps to stay safe, like tracking symptoms and attending follow-ups.
- Feel supported during recovery with guidance that helps you feel seen and heard.
What Is Postpartum Preeclampsia?

Postpartum preeclampsia is a condition where high blood pressure and signs of organ stress develop after childbirth. It usually shows up within 48 hours of delivery but can also occur up to six weeks postpartum, even if your pregnancy and labor were uneventful.
While it stems from the same condition, postpartum preeclampsia has a different timeline. And here’s something important to know: you don’t need to have had preeclampsia during pregnancy to develop it postpartum.
What’s happening? After birth, your body goes through massive shifts, hormones, blood flow, and fluid regulation. Sometimes, these changes can trigger blood pressure spikes and stress on your organs, like the liver or kidneys.
Postpartum preeclampsia isn’t common, but it’s serious and treatable, especially when caught early.
Why Postpartum Preeclampsia Awareness Matters
Postpartum preeclampsia isn’t something you need to fear, but it is something to keep on your radar. After all the physical and emotional effort of bringing your baby into the world, you deserve a recovery that feels safe and supported.
This condition can become serious if left untreated, sometimes leading to complications like:
- Seizures (eclampsia)
- Stroke
- Organ stress or failure: especially affecting the kidneys, liver, or heart
- Pulmonary edema: fluid buildup in the lungs that can cause breathing difficulty
- HELLP syndrome: a severe form of preeclampsia that involves hemolysis, elevated liver enzymes, and low platelet count
- Visual disturbances: including blurred vision or temporary loss of vision
- High blood pressure emergencies: may damage blood vessels and vital organs.
- Blood clotting issues: which can increase the risk of bleeding or thrombosis
But here’s the most important part: Most moms who receive timely care go on to recover fully. You don’t need to carry worry, just awareness. You don’t have to worry, you just need to be aware of the signs.
Risk Factors for Postpartum Preeclampsia

Postpartum preeclampsia can feel unexpected, especially when you’ve already made it through pregnancy and birth. While some mothers may have a higher chance of developing it, it’s important to remember that this condition can affect anyone, even without clear risk factors. That’s why gentle awareness matters more than worry.
You may be at a higher risk if:
- You had high blood pressure before or during pregnancy, as this can put added stress on your cardiovascular system even after delivery.
- You experienced preeclampsia while pregnant, which can sometimes extend into the postpartum period.
- There’s a history of preeclampsia in your family, or you’ve had it before, which may indicate a genetic or recurring tendency.
- You’re under 20 or over 40, as hormonal and vascular changes during these age ranges may increase your vulnerability.
- You carried multiples like twins or triplets, which places more physical demand on your body and circulatory system.
- You live with an autoimmune condition, such as lupus or antiphospholipid syndrome, which can affect how your body handles inflammation and clotting.
- You have Type 1 or Type 2 diabetes, which can impact blood vessel function and overall circulation.
- You had a cesarean birth, which may involve a more complex recovery and added strain on your body.
- You experienced significant weight gain during pregnancy or have a higher body weight, both of which can contribute to higher postpartum blood pressure.
- You received large amounts of IV fluids during labour, which can sometimes lead to fluid overload and affect your blood pressure balance after birth.
If some of these apply to you, it’s just a reminder to stay mindful of how you’re feeling. And if none of them apply, your body still deserves attention and care, because postpartum preeclampsia can happen without warning.
What to Watch For: Symptoms to Know
Some postpartum preeclampsia symptoms can feel confusing, especially when they overlap with normal recovery. That’s why having a clear reference can help. Here’s a quick guide to help you see when it might be time to reach out for help.
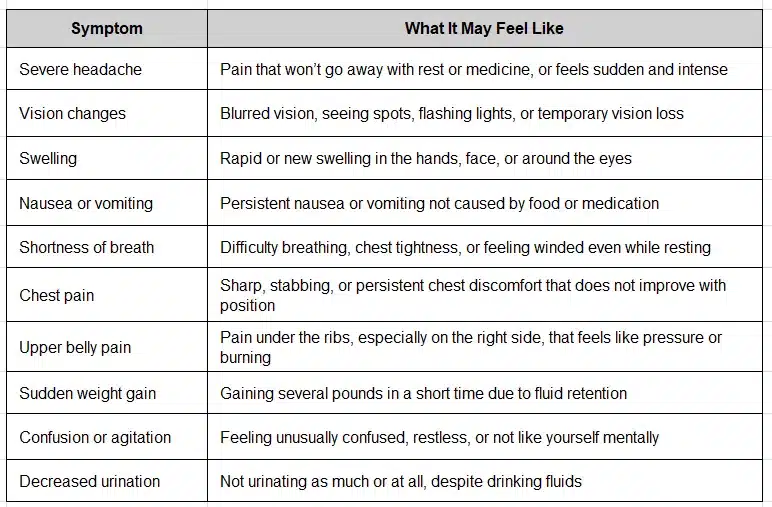
If something doesn’t feel right, trust that instinct. You know your body better than anyone.
Diagnosis and Treatment Steps for Postpartum Preeclampsia

If your healthcare provider suspects postpartum preeclampsia, they’ll carefully run tests to understand what’s happening in your body. These checks are just a way to make sure you’re okay and to find the best care for your recovery.
Here’s what diagnosis usually involves:
- Blood pressure check: This is often the first step. If your numbers are consistently high, it signals that your body might be under stress.
- Blood tests: Your doctor will look at your platelet count and check how your liver and kidneys are functioning. These organs can be affected when blood pressure rises.
- Urinalysis: This simple test checks your urine for protein, a key sign that your kidneys might be under pressure.
- Brain imaging (CT or MRI): In rare cases, especially if you’ve had a seizure or intense neurological symptoms, a scan may be done to check for any complications.
If you are diagnosed with postpartum preeclampsia, please know this: it is treatable, and with the right care, you can heal and feel better.
Most mothers are treated successfully with a combination of:
- Magnesium sulfate (IV): This helps prevent seizures and protects the brain.
- Blood pressure medications: These bring your pressure down to a safer range and reduce stress on your organs.
- Close monitoring: Sometimes this means a short stay in the hospital so your care team can respond quickly to any changes.
Recovery looks different for every mom, but many start to feel better within days. Some may need to continue medications or follow-up care for a few weeks or months, but the most important thing is that you are not alone, and you will be okay.
How to Stay One Step Ahead of Postpartum Preeclampsia

Taking care of yourself now is just as important, and it doesn’t have to feel overwhelming. A few gentle, proactive steps can go a long way in keeping you safe and supported during postpartum recovery.
Here’s what you can do:
- Schedule a follow-up blood pressure check: Within 7 to 10 days after delivery, especially if you had high blood pressure during pregnancy or birth.
- Check your blood pressure at home: If your doctor recommends it. Many pharmacies offer affordable monitors, and regular tracking can help catch early signs.
- Notice how your body feels: Severe headaches, vision changes, swelling in your hands or face, chest pain, or shortness of breath should not be ignored.
- Keep all postpartum appointments: Even if you feel fine. These checkups can help detect issues before they become serious.
- Speak up about unusual symptoms: If something feels off, call your doctor. Your concerns are always valid.
- Know your risk factors: A history of preeclampsia, gestational hypertension, obesity, or high blood pressure can raise your risk after childbirth.
- Ask loved ones to check in: Friends or family may notice changes like swelling, confusion, or fatigue that are easy to miss when you’re focused on your baby.
- Rest when you can and stay hydrated: Your recovery is important and deserves care and attention.
Final Words
It’s okay if your healing hasn’t gone exactly how you expected. Postpartum can be filled with beautiful moments, but also uncertainty, and that doesn’t make you any less strong. If you’re feeling off, worried, or simply not like yourself, that inner knowing deserves to be heard. You’re not alone in this, and you don’t have to manage it in silence.
You matter. Your recovery matters. And you deserve to feel safe and healthy.
Frequently Asked Questions
- Do I need to worry about postpartum preeclampsia if I had no issues during pregnancy?
Not always, but it’s good to be aware. Postpartum preeclampsia can happen even if you had a smooth pregnancy. Knowing the signs simply helps you feel more prepared, just in case. - How can I tell the difference between normal postpartum recovery and warning signs?
If something feels off, like a persistent headache, blurry vision, or swelling on hands or face that comes on suddenly, it’s worth checking in. You know your body best, and it’s okay to ask for help even if you’re unsure. - Will I need to stay in the hospital if I’m diagnosed?
Sometimes, especially if your blood pressure is very high or you need IV medication. But many cases are managed safely with monitoring and medication, and most moms recover well with the right support. - Can I still breastfeed if I’m being treated for postpartum preeclampsia?
Yes. Most blood pressure medications and treatments are safe while breastfeeding, but always check with your healthcare provider. - What can I do to lower my risk or catch it early?
Keep your follow-up appointments, track how you feel, and don’t ignore small changes. A quick blood pressure check in the first week after birth can be an important part of protecting your health.










